"I wasn't really thinking PE at first," they explained to me, "but after I saw the incomplete RBBB on the ECG, I sent a D-dimer." The D-dimer, of course, came back trivially elevated, and the CT had been ordered.
Ah, the scourge of the IRBBB. It typically take the appearance of an rSR' pattern in V1 and V2 with a narrow QRS, although the AHA takes a dim view of this colloquial definition.
This seemingly "hard" element of evidence, however, can be surprisingly malleable!
I cured the patient's IRBBB!
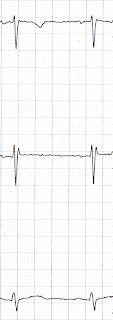
The patient was already off at CT, so I looked at the ECG myself. It looked pretty darn normal, except for the right-precordial leads:
V2 shows an rSR' pattern, clearly.
The patient returned from CT scan, and I awaited the results. In the meantime, however, I re-interviewed an examined the patient, and convinced myself that she was low risk for all of the "bad actors." The IRBBB stuck in my craw, however, and after some fiddling around, I aquired a new ECG.
Sweet. It's not up there with sinking a difficult tube, or threading a pacer wire, but it makes for a cleaner chart!
What did I do?
I put V1 and V2 where they are supposed to go.
For a fuller explanation of the background here, please check out The most difficult step in obtaining an ECG. It's a post I wrote for paramedics about the importance, as well as the common difficulty, of placing the precordial leads in the correct locations. It's written in a conversational and witty tone, with plenty of illustrations - you'll like it!
Suffice it to say, though, that V1 and V2 are usually placed far too high on the chest. This produces a number of artifacts, including pseudo-infarction patterns and, yes, IRBBB.
I took a picture (with the patient's knowledge and permission - she believes in education!) of the actual lead placements on the patient's chest. The electrode wires are attached to the proper locations, at the 4th intercostal spaces, just to the right and left of the sternum.
 |
| Thank you Ms Anonymous! |
The Bottom Line
Learn where to put the leads yourself.
If the diagnosis is going to rely critically on the ECG, you ought to check out where the electrodes were placed by the nurse, tech, or paramedic. Certainly, if there are abnormalities isolated to the precordial leads you should go back and do this, especially if the ECG doesn't match the patient's age or presentation.
BONUS QUESTION: For major extra points at the "Port, tell me what electrophysiologic diagnosis may rely on placing V1 and V2 higher than usual.
(Answer can be found by checking my self-aggrandizing link.)
*******
Added post-publication.
Mr Várhegyi points out a similar example, elsewhere on the web, of an IRBBB. Oddly, that example seemed to show some QRS prolongation in V2 that was not appreciated in the other leads.
 |
| Source |
So, I took another look at my patient's initial ECG:
Darned if it doesn't seem to also have an isolated, minor (< 0.02 seconds), QRS prolongation in V2.
I'm going to defer providing an explanation until I have some idea about why this occurs, or even declaring that this is a reliable feature of improperly placed precordial leads. But it's apparent in these two examples. I'll look into it - anyone else with a better idea write in!


Great post!
ReplyDeletePlacing V1 and V2 higher than usual may help identify the Brugada pattern.
Do anyone still doubt natural herbs? I've seen the great importance of natural herbs and the wonderful work they have done in people's lives. I wonder why people still spend their money on injections and drugs each time they are sick. Natural herbs can cure all kinds of illness including herpes, diabetes, asthma, HIV, HSV1&2, hepatitis, HPV etc. I've seen it with my own eyes. I was cured from Herpes and HPV and my aunt and her husband were cured from Hiv too by DR. Chukwu madu herbs. He uses natural herbs to cure different kind of virus. Dr. CHUKWU,prove to the world that natural herbs can cure all illness and he cured countless people using herbs. I know is hard to believe but am a living testimony. I was diagnose of Herpes and HPV in 2016 and i believe there is cure even when the doctors said there is no cure yet. I strongly believe in herbs and i came across a comment on a blog written by Lisa Pierre, saying she was cured from HERPES by Dr. CHUKWU MADU and i contacted his herbal hom on the email that was provided on the comment and order one for myself and he send it to me through UPS and gave me instructions on how to use it and after i finish taken it i went for checkup and the result shows am Herpes and HPV NEGATIVE. The doctor said that the virus is completely gone from my body. There is no harm trying herbs it work perfectly and it has no effect. You can contact Dr. CHUKWU MADU to get yours.. His email is dr.chukwumaduherbalhome@gmail.com.
DeleteWhatsApp +2347030936239.
THANX TO DOCTOR OSAZE WHO CURE ME FROM HERPES SIMPLEX AND cancer WITH HIS HERBAL MEDICATION, MY ENTIRE LIFE WAS BECOMING MISERABLE WHEN I CONTACTED THESE DIESEASES, I WENT TO DIFFERENT HOSPITAL IN NEWYORK AND CONNECTICUT TO NO AND VAIL, UNTIL I CAME ACROSS DOCTOR OSAZEE'S TESTIMONIES ONLINE ON HOW HE HAS BEEN USING HIS HERBS TO CURE PEOPLE OF HERPES DIESEASES, AND I DICIDED TO CONTACT HIM AND GIVE HIS MEDICATION A TRY, WITHIN ONE MONTH AND A WEEK I WAS TOTALLY CURED, IN CASE YOU ARE GOING THROUGH SIMILAR PROBLEM AND YOU WANTS TO CONTACT DR OSAZEE, YOU CAN EMAIL HIM ON: DROSAZEHERBAL@GMAIL.COM OR CALL OR WHATSAP HIM ON: +2347089275769
DeleteI want to write a little testimony about the good work of doctor ehiaguna who cured me from Hsv 1 and 2 for just 2 week with his herbal medicine, I never believe I can be normal again and have a good life like others I always regretted the day I got diagnose with the virus, I was lost of hope when my doctor told me there is no cure for it but I keep thinking and thinking about my future, if I can have kids of my own well I am so grateful for my helper who get me cured with his herbal medicine, I go online in search of anything that can help me because I can’t deal with it forever so I found this Dr ehiaguna email on a Facebook of someone who was cured by him I quickly contact him for help and explain all my pain to him, he told me not to worry about it there is cure for real, I never believe until he send me the herbal medicine when I order for it and I have it within 4 days that is how I took the medicine for 2 week and the following week I go for test just to confirm I was 100% cured from this sickness what a miracle in my life I am so happy right now, you can also get in contact with him if you have such sickness through drehiaguna@gmail.com and also WhatsApp him +2348073908953. he can also help with this following sickness DIABETES CURE/EPILESY/HPV/CURE/LUPUS/HEPATITIS
DeleteGood day to you all am very happy to write this testimony to the whole world to see the great work of the great man named DR.ehiaguna I was down over since 1year but thank god am here to give this testimony for you all to see the great powers that is hiding on this earth I was once an HSV 2, but thanks to him that help me I was going through internet looking for cure when I see this man name ehiaguna I quickly email him If I can get help to grateful surprise to me he really do according to the post I see on internet this man ask me to provide some necessary things which he should be able to use for my cure, I did what he say and after everything, this man told me that after two weeks I will be cured, after that ending of the weeks i should go for test I did and I was very happy when I see my result but i don’t know how he did it but thank God for bring this man to me am very happy to see myself am HSV negative you can order now and get your cure on email: drehiaguna@gmail.com just call him for quick answer on his number +2348073908953, also contact him on this 1. HIV / AIDS 2. COPD 3. CANCER 4. ALS (Lou Gehrig's disease) 5. Hepatitis B6. HPV
DeleteBEST NATURAL TREATMENT FOR HUMAN PAPILLOMAVIRUS (HPV) earning that you have HPV can be one of the most difficult experiences you go through in life. You may feel scared, sad or even angry – this is OK, and a completely natural part of coping with something that can be life changing.
DeleteIt will probably take a while for the news to sink in.
My name is Johnny Mary and i am from the United States.
I remember spending so much money buying drugs from hospitals hoping that i will be cured from HPV VIRUS, but all to no avail. I contacted so many doctors and they prescribe medicine for me which they indeed tried their best but was unable to provide for me a possible cure, luckily i saw a comment about a herbal doctor, (Dr.Ogberaese) online.
I then contacted him (Dr.Ogberaese) through his email, After much chat and enquiry with the doctor, i decide to take a leap of faith because i have nothing to loose.
To my greatest surprise, Dr.Ogberaese prepare a medicine and send me a Herbal Medicine through FEDEX courier Service, and he gave me guidelines on how am to take it. I followed all procedures as instructed, and after 2 weeks of taking it i was cure from HPV VIRUS his medicine is legit and it is real. I just want to encourage all individuals out there living with HERPES , ITCHY SHINGLES , Genital Herpes, HSV1&2, HIV/AIDS/ HPV, COPD, CANCER, Hepatitis b, Lupus, PCOS, Kidney failure, Lung cancer and alot more. That there is still a huge chance that you can get cure only with the help of dr Ogberaese. kindly contact him via email: drogberaese54@gmail.com or whatsapp: +2348073818653
I want to give a testimony on how I was cured from herpes ii virus after using Doctor Patrick liquid herbal medicines for one month only, i found about Doctor Patrick on newspaper, I had to take his email and phone number and then contacted him, I explained everything to him and he assured me that he can help me and I will be free from this infection forever. He sent me the medicines and I started using according to his instructions, after two weeks of using the medicines, I saw great changes, I continued using the medicine until I used it all for one month, I was cured totally, no more symptoms and I went for another diagnosis, the Doctor gave me my test result and it came out negative, I want to thank God for making this come true and I want to thank Doctor Patrick for what he has done for me, contact this herbal doctor on herbalmedicalhome@gmail.com and whatsApp number is +2348021312463.
DeleteI never believed that their could be any complete cure for Herpes 2, Mrs JANE introduce me to DR.ehiaguna a herbal doctor, who brought him back to life again. so i had to try it too and you can,t believe that in just two weeks i started using the herbal medicine he sent to me i was perfectly ok and . Right now i can tell you that few months now i have not had any symptoms of Herpes and i have just went for text last week and the doctor confirmed that there is no trace of any Herpes in my body system. Glory be to God for leading me to this genuine DR.ehiaguna I am so happy as i am sharing this testimony. My advice to you all who thinks that their is no cure for HSV that is Not true ,just contact him and get cure from DR.ehiaguna via his Email drehiaguna@gmail.com and you will be free and free forever, Try it and you will not regret it because it truly works. One thing i have come to realize is that you never know how true it is until you try...email him drehiaguna@gmail.com.. OR WhatsApp +2348073908953 THIS IS THE TYPE OF HERBAL MEDICATION HE HAVE1 Cancer 2 Hiv 3 Low sperm count 4 Barrenness 5 Hvp 6 Herpes 7 Genital Wart 8 Rare disease 9 Hepatitis 10 Syphilis 11 DiabetesGod bless you sir for your good work that you done.....
Deletefew week ago I felt some pains and I went to the hospital my doc told me I had Herpes about 1 year ago and I need to start the treatment early, he gave me some medicine to be taking and I told him no I’ll not, because I hated taking medicine when I won’t not see cure for the purpose. After I got home I started getting worried searching for strong advice and I found valid natural treatment online a lot of people says they got herpes cure from DR ehiaguna and I contacted DR ehiaguna that same day I purchase his cure online, after two weeks of taking the herbel treatment i got cured totally. i tested negative all thank to DR ehiaguna you can also reach him on his email: [drehiaguna@gmail.com ] or message him on WhatsApp +2348073908953 God bless you
DeleteExcellent! Grabbing the early-morning bonus points.
ReplyDeleteDear Dr. Walsh!
ReplyDeleteYesterday on one of the ECG pages on Facebook a similar case was posted. Maybe you have already read that.
The ECG is here (with my modification):
http://kepfeltoltes.hu/view/121222/Brugada_or_too-high-lead-placement_www.kepfeltoltes.hu_.jpg
I was totally certain that this is not RBBB, because:
1. There is no deep and wide S wave in left sided leads.
But more interesting:
2. There is an isolated QRS prolongation in V1-2 (QRS is 120 ms wide in V1-2, but about 90-100 ms in other leads). On the ECG linked above I put a vertical line through the J point of V3, and so one can see that the QRS ends at the top of the R' wave in V1-2, so these are not R' waves actually, and that is why the top of them is the J point itself, and the QRS is not 120 ms wide as we think if we only see V1-2, but 90-100 ms (as in V3 and other leads).
And if that is the J point then the ST segment is by definiton elevated (so it is a downsloping ST elevation).
That's (downsloping ST elevation) why I thought it is Brugada pattern which was supported by the patients history of cocaine abuse (which - as far as I know - can mimick or trigger the appearance of Brugada pattern). However, not so typical Brugada pattern, as the ST segment is only elevated for 20 ms.
BUT:
The admin then wrote the solution: V1 and V2 were placed too high.
I know this can cause RBBB-like pattern, but I think it won't cause QRS prolongation, especially isolated QRS prolongation in V1-2. So I'm a bit skeptic:-)
In your example here the QRS is not prolonged (comparing the wrong and the right lead placement strip, the QRS is about 80 ms in both).
What do you think?
Thanks for your answer!
Best regards,
Márton Várhegyi
5th year medical student
Semmelweis University, Hungary
(interested in electrocardiography and emergency medicine)
This is interesting. I have had numerous ecg's. Everytime I have a episode of getting dizzy, and heart racing. I am 38 year old female. I don't think they placed them the way you are saying, in fact I know they didn't. So they are saying I have a incomplete rbbb. They just want to put me on a beta blocker to stop heart racing . It gets bad that it wakes me out of sleep. Makes me feel really drained after wards and I shake uncontrollablly for a few mins. Two months ago I was running, riding a bike an such!5129069040. Really find your information interesting!
ReplyDeleteHello! I just needed to thank you for this post! I am a microbiologyst, 41 y.o. and I was diagnosed by routine check with IRBBB of course by 2 cardiologysts colegues but reading your posts I began to smell something rotting 😁 I repeated the 3-rd EKG with correct V1,2 electrodes and so beeing cured by this infamous condition in just a weekend! THANKS !!!
ReplyDeleteThis is a fantastic and great, doc!
ReplyDeleteI am so impressed and thanks for sharing this info.
God bless
PS.
ReplyDeleteI hope that more people like you who will spread great news and info without any charges...
Do anyone still doubt natural herbs? I've seen the great importance of natural herbs and the wonderful work they have done in people's lives. I wonder why people still spend their money on injections and drugs each time they are sick. Natural herbs can cure all kinds of illness including herpes, diabetes, asthma, HIV, HSV1&2, hepatitis, HPV etc. I've seen it with my own eyes. I was cured from Herpes and HPV and my aunt and her husband were cured from Hiv too by DR. Chukwu madu herbs. He uses natural herbs to cure different kind of virus. Dr. CHUKWU,prove to the world that natural herbs can cure all illness and he cured countless people using herbs. I know is hard to believe but am a living testimony. I was diagnose of Herpes and HPV in 2016 and i believe there is cure even when the doctors said there is no cure yet. I strongly believe in herbs and i came across a comment on a blog written by Lisa Pierre, saying she was cured from HERPES by Dr. CHUKWU MADU and i contacted his herbal hom on the email that was provided on the comment and order one for myself and he send it to me through UPS and gave me instructions on how to use it and after i finish taken it i went for checkup and the result shows am Herpes and HPV NEGATIVE. The doctor said that the virus is completely gone from my body. There is no harm trying herbs it work perfectly and it has no effect. You can contact Dr. CHUKWU MADU to get yours.. His email is dr.chukwumaduherbalhome@gmail.com.
ReplyDeleteWhatsApp +2347030936239.
My joy knows no bounds, I never thought that one day I will live on earth cured of this virus. I have been suffering from this deadly virus "HERPES SIMPLEX VIRUS" since 5 years ago. I have spent a lot of money on drugs and going from one hospital to another, hospital has been my most visited place where constant check up have been my hobby not until one day, i decided to share my situation to a very close friend of mine and she was very upset with me for not telling her ever since that she is aware of one doctor called Dr. Sani who helps people in curing their HERPES. quickly i contacted his email: perfectherbalcure@gmail.com that was given to me by Carolyn, just to give him a test, i spoke to him, he asked me to do some certain things which i did, he told me that he was going to prepare and send some herbal cure to me, which he did and thereafter i received it and after using the herbal cure within 2weeks and few days i was totally cured, i had to go back to the same hospital that I have been going before to confirm my cure and behold I was confirmed negative by my doctor, so today I am here to spread the good-news of my life on how Dr. Sani saved me from the nightmare and outbreaks of HERPES VIRUS. You can contact him via email: perfectherbalcure@gmail.com or Whats-app: +2348118184266. If you are still suffering from this deadly virus...I believe you're going to be happy and feel alive again just as I am right now.
ReplyDeleteEmail: perfectherbalcure@gmail.com
Whats-app: +2348118184266
I'm Celina Gomez from Canada, i have been cured from genital herpes with herbalist Sakura herbal Remedy.
ReplyDeletei have been infected with genital herpes for 1 years now , i have done so many medical treatments from different hospitals still
not cured. On a very good day , I decided to do research on my computer on how to get rid of genital herpes,i found a post of Sarah Wilson on how she was cured from herpes with herbalist Dr sakura herbal remedy.
The Herbalist email/contact number was there as well dr.sakuraspellalter@gmail.com/ +2348160802189. I contacted him because of my illness .He needed few of my information which i did, and also sent me his medicine through FedEx courier service.
which i received after 3 working days of shipment,i drink the herbal medicine the same way Herbalist Dr Sakura instructed me too.but now my genital herpes is gone totally without any side effect or harm, may God Almighty continuing to bless him abundantly .
you can contact him on mail/whats app dr.sakuraspellalter@gmail.com +2348110114739 or follow him on Instagram @Herbalist_sakura .you can also mail me for more information celinagomez784@gmail.com
I was cured from HEPATITIS B VIRUS with the used of natural herbs. My name is Mark a 35-yrs old man from the USA. I love herbs so much. Most times, injection and drugs are just a waste of time. I was cured 6months ago, i suffered from HEPATITIS B VIRUS for years but with the help of Dr Oseremen herbal medicine, i was cured within few weeks of drinking the herbs he sent to me through courier delivery service. This same doctor also cured my Aunty from herpes, as soon as i heard she had herpes, i quickly refer her to Dr Oseremen and she was cured too after drinking his herbs.I have referred more than 15 persons to Dr Oseremen and they were all cured from their various illness. Have you taken herbs before?. You have spent so much money on drugs,injections,surgeries etc and yet you have no good result to show for it. Contact Dr Oseremen now, he is a herbalist doctor, i assured you of a cure if you drink his natural herbs. Dr Oseremen have herbs that cures+HIV+Herpes+Diabetics+Asthma+Hepatitis+HBP+STD+Cancer+Chronic etc.He is also a spell caster, he can cast a spell to bring back your EX lover. Contact Dr Oseremen through his WHATSAPP +2349056394313 or Email address Dr.Oseremenvadi@gmail.com Share the good news to others once you are cured. Thank you
ReplyDeleteCan't still believe that i got cured from Genital Herpes through herbal treatment from Dr Ebhota who I met through the internet, I actually couldn't believe it at first because it sounded impossible to me knowing how far I have gone just to get rid of it. Dr Ebhota send me his medicine which I took as instructed and here I am living a happy life once again, a big thanks to Dr Ebhota , I am sure there are many herbal doctors out there but Dr Ebhota did it for me, contact him drebhotasolution@gmail.com , also call or whatsApp him on +2348089535482
ReplyDeleteMy health was horrible before I decided to try the Protocol Of taking Dr. Omola pure herbal mixture. I felt there was no hope for my health and I was to try the Protocol, thinking it wouldn’t work because I have visited so many hospital but same result. However, I was convinced by a Instagram friend to try the herbal medicine because I wanted to get rid of Herpes virus. The herbal mixture that was given to me was really quick and easy to take, within 2 week I was fully cured from Herpes. The herbal medicine really work and I will like to share this great doctor contact with you all email him dr.omolaherbalhome@gmail.com or WhatsApp +2348118116254 you won't regret it, I promise.
ReplyDeleteFINALLY FREE FROM HERPES VIRUSI thought my life had nothing to offer anymore because life became meaningless to me because I had Herpes virus, the symptoms became very severe and bold and made my family run from and abandoned me so they won't get infected. I gave up everything, my hope, dreams,vision and job because the doctor told me there's no cure. I consumed so many drugs but they never cured me but hid the symptoms inside me making it worse. I was doing some research online someday when I Came across testimonies of some people of how DR Ebhota cure them from Herpes, I never believed at first and thought it was a joke but later decided to contact him on the details provided and when I messaged him we talked and he sent mehis herbal medicine and told me to go for a test after two weeks. Within 7 days of medication the symptoms disappeared and when I went for a test Lo and behold I was NEGATIVE by the Doctor Who tested me earlier. Thank you Dr Ebhota because I forever owe you my life and I'll keep on telling the world about you. If you are going through the same situation worry no more and contact DR Ebhota viadrebhotasolution@gmail. com or WhatsApp him via +2348089535482.he also special on curing 1. HIV/AIDS2. HERPES 3. CANCER 4.ALS 5. HEPATITIS B 6.DIABETES 7. HUMAN PAPILLOMAVIRUS DISEASE(HPV)8. ALZHEIMER 9. LUPUS (Lupus Vulgaris or LupusErythematosus
ReplyDeleteFor years, I have read and seen the advertisements in the mass media about all of the penis enhancement pills and thought that they were all scams or gimmicks. All of the medical sites that I have visited stated that none of the herbal supplements would ever help increase the size of a penis. I got very depressed when I read this, because unfortunately I was not naturally blessed with a penis that was big enough to arouse my sexual partner or past partners. I am a man that is past my sexual prime time and my sexual performance has a lot to be desired. I decided to try Doctor Akhigbe herbal medicine after all the reading and researching that I have done.I saw a testimony " Joe" about doctor Akhigbe Herbal Medicine Since there is a Money Back Guarantee, I give him a trial what did I have to lose? I couldn't believe the results I was seeing after drinking the Natural Herbal Medicine and Herbal Soap to be Rubin my penis! he sent to me through DHL courier delivery service . Within about 2 weeks I had a noticeable increase in the girth of my penis. Then after a couple of additional week it started to grow in length and I was amazed and very excited.before I finish the drink and the soap my penis had grown an additional two inches. I've had a considerable improvement with my sex life and these pills are certainly worth every penny I spent on them! I want to thank Dr Akhigbe for the time and effort they have spent on helping people in my situation.I know many are out there who are suffering this problem and they need help, email him. drrealakhigbe@gmail.com. He also cure other diseases like: Painful or Irregular Menstruation. HIV/Aids. Breast Enlargement. Diabetics. Vaginal Infections. Vaginal Discharge. Itching Of the Private Part. Breast Infection. Discharge from Breast. Breast Pain & Itching. Lower Abdominal Pain. No Periods or Periods Suddenly Stop. Women Sexual Problems. High Blood Pressure Chronic Disease. Pain during Sex inside the Pelvis. Pain during Urination. Pelvic Inflammatory Disease, (PID). Dripping Of Sperm from the Vagina As Well As for Low sperm count. Parkinson disease. Lupus. Cancer. Tuberculosis. Zero sperm count. Asthma. Quick Ejaculation. Corneal Ulcer, Gallstone, Terminal Illnesses, Premature Ejaculation. Herpes. Joint Pain. Stroke. Weak Erection. Erysipelas, Thyroid, Discharge from Penis. HPV. Impotence Effection, Hepatitis A and B. STD. Staphylococcus + Gonorrhea + Syphilis. Heart Disease. Pile-Hemorrhoid.rheumatism, thyroid, Autism, Penis enlargement, Waist & Back Pain. Male Infertility and Female Infertility. For your cure email him now: drrealakhigbe@gmail.com or Contact his number: +2349010754824.
ReplyDeleteHELLO everyone! Still don’t know the right words to express my Gratitude to the Great DR.Imoudu After been diagnosed with the #herpes for the passed 1 years, i was given so many health prescription and advice with no improvement, I totally lost hope, until i found many testimonies of Great DR.Imoudu in an online research Like anybody would be, i advice anyone that is living with herpes can also contact him today, because he has the cure to any virus problem contact him on WhatsApp +2348109609753..
ReplyDeleteOr his Email: DR.IMOUDUHEALERTEMPLE@GMAIL. COM
1...ALS CURE/DIABETES CURE/EPILESY/HPV CURE/LOOSE WEIGHT AND BODY/EX-BACK/HEPATITIS/
THANK YOU DR.Imoudu FOR YOU GOOD WORK IN MY LIFE..
I’m here to testify about what Dr. Omola did for me. I have been suffering from (GENITAL HERPES VIRUS) disease for the past 3 years and had constant pain and inching, especially in my private part. During the first year, I had faith in God that i would be cured someday.This disease started circulating all over my body and I have been taking treatment from my doctor, few weeks ago I came across a testimony of Mary on the internet testifying about a Man called Dr. Omola on how he cured her from 5 years HSV 2. And she also gave the email address of this man, advise anybody to contact him for help on any kind of diseases that he would be of help, so I emailed him telling him about my (HSV 2) he told me not to worry that I was going to be cured!! Well, I never doubted him I have faith he can cure me too,, Dr. Omola prepared and sent me Healing Oil, Soap, roots and herbs which I took. In the first one week, I started experiencing changes all over me, after four weeks of using his Roots/ Herbs, Oil and Soap, I was totally cured. no more inching , pain on me anymore as Dr. Omola assured me. After some time I went to my doctor to do another test behold the result came out negative. So friends my advise is if you have such disease or know anyone who suffers from it or any other disease like HPV, HBV, HIV, ALS, HBP, CANCER etc. you can contact Dr. Omola for help via dr.omolaherbalhome@gmail.com or whatsapp +2348118116254.
ReplyDelete𝙊𝙧𝙖𝙡 𝙝𝙚𝙧𝙥𝙚𝙨 𝙞𝙨 𝙖 𝙗𝙤𝙩𝙝𝙚𝙧𝙞𝙣𝙜 𝙫𝙞𝙧𝙪𝙨, 𝘽𝙪𝙩 𝙤𝙫𝙚𝙧𝙘𝙤𝙢𝙞𝙣𝙜 𝙞𝙩 𝙞𝙨 𝙣𝙤𝙩 𝙞𝙢𝙥𝙤𝙨𝙨𝙞𝙗𝙡𝙚 𝙖𝙣𝙮𝙢𝙤𝙧𝙚!
ReplyDelete𝙈𝙨. 𝙏𝘼 𝙛𝙧𝙤𝙢 𝙩𝙝𝙚 𝘼𝙐𝙎𝙏𝙍𝘼𝙇𝙄𝘼 𝙬𝙖𝙨 𝙙𝙞𝙖𝙜𝙣𝙤𝙨𝙚𝙙 𝙬𝙞𝙩𝙝 𝙜𝙚𝙣𝙞𝙩𝙖𝙡 𝙝𝙚𝙧𝙥𝙚𝙨 𝙩𝙮𝙥𝙚1 (𝙃𝙎𝙑1), 𝙖𝙣𝙙 𝙨𝙝𝙚 𝙘𝙝𝙤𝙨𝙚 # 𝙙𝙧𝙪𝙩𝙪𝙝𝙚𝙧𝙗𝙖𝙡𝙘𝙪𝙧𝙚@gmail.𝙘𝙤𝙢 𝙛𝙤𝙧 𝙩𝙧𝙚𝙖𝙩𝙢𝙚𝙣𝙩 𝙬𝙝𝙚𝙧𝙚 𝙞𝙣 𝙨𝙝𝙚 𝙝𝙚𝙖𝙧𝙙 𝙖𝙣𝙙 𝙧𝙚𝙖𝙙 𝙖𝙗𝙤𝙪𝙩 𝘿𝙧 𝙐𝙩𝙪 𝙤𝙣 𝙖 𝙛𝙤𝙧𝙪𝙢. 𝘼𝙛𝙩𝙚𝙧 𝙛𝙤𝙪𝙧 𝙬𝙚𝙚𝙠𝙨 𝙢𝙚𝙙𝙞𝙘𝙖𝙩𝙞𝙤𝙣 𝙨𝙝𝙚 𝙬𝙚𝙣𝙩 𝙛𝙤𝙧 𝙩𝙚𝙨𝙩 𝙖𝙣𝙙 𝙬𝙖𝙨 𝙩𝙚𝙨𝙩𝙚𝙙 𝙣𝙚𝙜𝙖𝙩𝙞𝙫𝙚 𝙤𝙛 𝙝𝙨𝙫1. 𝘼𝙛𝙩𝙚𝙧 𝙝𝙚𝙖𝙧𝙞𝙣𝙜 𝙝𝙚𝙧 𝙩𝙚𝙨𝙩𝙞𝙢𝙤𝙣𝙮 𝙄 𝙜𝙖𝙫𝙚 𝙞𝙩 𝙖 𝙩𝙧𝙞𝙖𝙡 𝙖𝙣𝙙 𝙬𝙖𝙨 𝙘𝙤𝙢𝙥𝙡𝙚𝙩𝙚𝙡𝙮 𝙘𝙪𝙧𝙚𝙙
I was diagnosed of HERPES Virus in 2017 and I have tried all I can to get cured but all to no avail, until i saw a post in a health forum about a herbalist man who prepare herbal medication to cure all kind of diseases including HERPES virus, at first i doubted if it was real but decided to give it a try , when i contact this herbalist and he prepared a HERPES herbal cure and sent it to me via FEDEX delivery company service, when i received this herbal cure, he gave me step by directions on how to apply it, when i applied it as instructed, i was totally cured of this horrible disease within 17days of usage, i went to the hospital for a test and it was negative. I can tell to the public now that am now free from the horrible disease called herpes, all thanks to Dr.Ebhota that is why I want to leave his email address and What's app contact just if you want to contact him for help. you reach this great herbal doctor via his email on (drebhotasolution@gmail.com)website on: https://drebhotasolution.wixsite.com/drebhotaherbalhome / One thing I like about Dr Ebhota is honesty. His very polite with his customers, everything he told me was what he did. His herbal medicine are very affordable, effective, confidential.
ReplyDeleteI’m here to testify about what Dr. Omola did for me. I have been suffering from (GENITAL HERPES VIRUS) disease for the past 3 years and had constant pain and inching, especially in my private part. During the first year, I had faith in God that i would be cured someday.This disease started circulating all over my body and I have been taking treatment from my doctor, few weeks ago I came across a testimony of Mary on the internet testifying about a Man called Dr. Omola on how he cured her from 5 years HSV 2. And she also gave the email address of this man, advise anybody to contact him for help on any kind of diseases that he would be of help, so I emailed him telling him about my (HSV 2) he told me not to worry that I was going to be cured!! Well, I never doubted him I have faith he can cure me too,, Dr. Omola prepared and sent me Healing Oil, Soap, roots and herbs which I took. In the first one week, I started experiencing changes all over me, after four weeks of using his Roots/ Herbs, Oil and Soap, I was totally cured. no more inching , pain on me anymore as Dr. Omola assured me. After some time I went to my doctor to do another test behold the result came out negative. So friends my advise is if you have such disease or know anyone who suffers from it or any other disease like HPV, HBV, HIV, ALS, HBP, CANCER etc. you can contact Dr. Omola for help via dr.omolaherbalhome@gmail.com or whatsapp +2348118116254.
ReplyDeleteI want to thank Dr Ebhota, Herpes. Medicine is a good herbal medicine for the HERPES virus. I was diagnosed with the HERPES virus last month, and was looking for a solution to cure. Fortunately, I saw a testimony about how Dr Ebhota, CURE HERPES VIRUS I decided to contact Dr Ebhota,I contacted him He prepared a portion of herbal medicine and sent it to me, I started herbal medicine for my health. He gave me step by step instructions on how to apply it, when I applied it as instructed, I was cured of this deadly herpes virus within 2 weeks, now I am negative Ebhota . My brother and sister I do not know that there are so many people who have the same herpes virus, please Dr. Ebhota to help him too, and help me to thank Dr Ebhota for healing me, I am cured by Dr. Ebhota Medicine, his email Contact: drebhotasolution@gmail.com OR Cell Whatsapp Number +2348089535482. Dr Ebhota also has the cure for, psoriasis, cancer, HPV may God bless you sir for your good works.
ReplyDeleteMy God will continue to bless you more abundantly, for the good works you are doing in peoples life, I will keep on writng and posting testimonies about you on the Internet, I was a HSV patient, I saw a post on blog on how Dr. Omola cured someone, I contacted him and also got my healing, kindly email him now on dr.omolaherbalhome@gmail.com or His Whatsapp number: +2348118116254...thank you for the good work
ReplyDeleteDr Omola CAN AS WELL CURE THE FOLLOWING DISEASE:-LUPUS, CANCER, HBV, HPV, BARENESS/INFERTILITY, DIARRHEA,FIBROIDS, DIABETES, URINARY TRACT INFECTION, IMPOTENCE.
ReplyDeleteGreetings to the general public, i want to inform the public how i was cured of HERPES Simplex Virus by a Doctor called Dr. Omola i visited different hospital but they gave me list of drugs like Famvir, Zovirax, and Valtrex whicmptoms and never cured me. I was browsing through the Internet searching for remedy on HERPES and i saw comment of people talking about how Dr. Omola cured them. when i contacted him he gave me hope and send a Herbal medicine to me that i took and it seriously worked for me, i am a free person now without problem, my HERPES result came out negative. I pray for you Dr. Omola God will give you everlasting life, you shall not die before your time for being a sincere and great man. Am so happy, you can also contact him if you have any problem, Email Address dr.omolaherbalhome@gmail.com or whatsapp or call him +2348118116254. thank me later.
My health was horrible before I decided to try the Protocol Of taking Dr. Omola pure herbal mixture. I felt there was no hope for my health and I was to try the Protocol, thinking it wouldn’t work because I have visited so many hospital but same result. However, I was convinced by a Instagram friend to try the herbal medicine because I wanted to get rid of Herpes virus. The herbal mixture that was given to me was really quick and easy to take, within 2 week I was fully cured from Herpes. The herbal medicine really work and I will like to share this great doctor contact with you all email him dr.omolaherbalhome@gmail.com or WhatsApp +2348118116254 you won't regret it, I promise.
ReplyDeleteI have be living with Oral herpes for over 4 years now and it has be a big problem for me.I have been looking for solution because i can't leave with it, One day i came across a woman testimony on a forum saying she got cured of her Herpes with the help of Dr Ojamo an herbal doctor from African with herbal medicine. At first i did not believe because i was not sure herbs can really take this virus away,but i have no choice than to give it a try and contacted him with his emails, i explain my problems,.. then he told me not to worry that he will prepare the a cure with herbal mixture and send it to me, i got the medicine after 4 days delivery and i use as instructed. After 21 days when the herb got almost finish i went to a medical doctor, i did a test and discover that the virus was gone, and my test result were HSV 1%2 negative,i was so surprise and happy! then i wrote Dr Ojamo and thank him for getting me cured from herpes. I advice you to contact this great herbal doctor Ojamo as he have cure for different kinds of diseases.i decided to share this testimony to let others who also suffer from herpes know about this and give hope to others, you can reach him via Email dr.ojamoherbalhome@gmail.com WhatsApp number +2349077406037
ReplyDeleteYou can check on his website for more info
https://drojamoherbalhome.wixsite.com/welcometodrojamoherb
Finally I am free from herpes virus, with the help of Dr.Omola pure herbs, This Virus appeared at the age of 29, with no hope of a cure from the hospitals i have went to, I thought my life have come to an end, until a Facebook friend of mine told me about Dr. Omola who treats all Kinds of diseases including Herpes, I contacted him via his email: dr.omolaherbalhome@gmail.com, I explain everything to him so he ask for my home address, after telling me the cost of the herbal medicine so we agree at a particular price, he prepare the herbs and make delivery to me via FedEx delivery service they deliver the herbs to my door step, I drink the herbs as him instructed, I went for test in 3 different hospital and it was negative, today I'm free from herpes virus.
ReplyDeleteYou should try Dr.omola herbs I'm not the first person to be cured with his herbs there are different testimony about this herbal doctor, your case can not be different, here is his WhatsApp No +2348118116254 email: dr.omolaherbalhome@gmail.com.
Dr. Riaria cured my herpes virus that have been in my body since two years, ever since then my life has been incomplete, I have used so many drugs that was prescribed to me by doctors, but it didn't cure my herpes virus, i was checking for solution on the internet then I miraculously came across Dr. Riaria the powerful herbalist that can cure herpes infection, then I contacted him through his email, I explained everything to him and he prepared a herbal medicine and sent it to me through FedEx, which I took for 14 days with the instruction he gave me, and when I did a test in the hospital my result came out negative it was the happiest day of my life that am cure from HSV 2, are you also suffering from same virus or another diseases you can simply contact him via email: drriaria@gmail.com you can also call or WhatsApp him on: +2349134987375.
ReplyDeleteHOW ME AND MY FAMILY WAS TOTALLY CURED FROM COPD,CHRONIC PANCREATITIS,IDIOPHATIC PULMONARY FIBROSIS,
ReplyDeleteI was diagnosed of COPD disease in January 2014,then my mom, diagnosis of IDIOPATHIC PULMONARY FIBROSIS(IPF) and my father was diagnosed of CHRONIC PANCREATITIS.. Me and my family were so frustrated till one day my father came across a forum where so many people were writing about Dr Ovie, a herbal Dr, who sell herbal medicines to cure all kinds of diseases, We contacted this herbal doctor via his email ovie.miraclemedicine1@gmail.com and bought herbal medicine from him. He sent it to me through courier service and I received it within 2days. i used it as instructed and i and my family was totally cured of those disease within 30days of usage, all thanks to Dr Ovie.is three months now we are living free and happy, please viewers this testimony is real …call or whats app Dr Ovie on +2349056393169
Dr Oduku herpes treatment is one of the most effective home remedies for herpes which has the ability to kill the herpes virus permanently. I found out I had herpes 4 years ago. My first outbreak was definitely the worst thing I ever experienced. The bumps and blisters were swollen and red. I had a doctor give me Valtrex but I take the generic. I had to take the Valtrex 1 gram a day for about a week and I had another doctor prescribe me Acyclovir but that gave me the worst headaches ever, so I stopped taking it.after 2 year all that prove abortive the herpes was still there,Since I was first diagnosed I have about 2 outbreaks a month. I have been able to cope with this by having supportive family and friends who look out for me,though it wasnt easy for me, one day i read a post by someone testifying about Dr Oduku that she was cured totally using his herbal product, i decided to gave it a try, I contacted him as instructed in the testimony. i made request for the herbal medicine, he actually did send it to me and gave me the instruction on how i will use it,The good news is this, i went to the hospital after the medication for test as instructed by Dr Oduku, i was tested negative, i was suprised finding out that am now herpes virus negative against my former result which was positive, Am happy to let the whole world know that today am free from this herpes disease,no more outbreak, no more cold sores, excruciating pains, i will advice anyone reading this message and needed a cure for herpes as well should please contact this Great Dr Oduku on drodukuherbalhealingcentre@gmail.com or WhatsApp +2348124765093
ReplyDeleteVisit his website: https://dr-oduku-herbal-healing-centre.jimdosite.com
https://drodukuherbscure.blogspot.com/
Dr Oduku is the best herbal doctor.
Here is my private e-mail clararose2128@gmail.com you can also get in touch with me.,,,,,,....
This is real take it serious, who will believe that a herb can cure HERPES DISEASE in my body, i never believe that this will work i have spend alot when getting drugs from the hospital to keep me healthy, what i waswaiting for is death because i was broke, one day i hard about this greatman who is well know of HIV,cancer and herpes cure, i decided to email him,unknowingly to me that this will be the end of the HERPES DISEASE, heprepare the herb for me, and give me instruction on how to take it, at theend of the week which was seven days,he told me to go to the hospital for acheck up, and i went surprisingly after it the doctor confirm me cure fromHERPES disease I thought it was a joke, i went to other hospital the doctorthere also confirm me cure from HERPES disease then i took my friend whowas also HERPES patient to the Doctor after the taking of the herbs she wasalso confirm cure from HERPES disease .please I want every one with thisvirus to be free, that is why am dropping his email address,(drodukuherbalhealingcentre@gmail.com or his whatsap contact +2348124765093)you can visit his website https://drodukuherbscure.blogspot.com/or his blogs pagehttps://dr-oduku-herbal-healing-centre.jimdosite.com/i want you to email him he is a great man. thank you for saving my life, and I promise Iwill always testify for your good work. you can also reach me clararose2128@gmail.com
ReplyDeleteI want to write a little testimony about the good work of doctor ehiaguna who cured me from Hsv 1 and 2 for just 2 week with his herbal medicine, I never believe I can be normal again and have a good life like others I always regretted the day I got diagnose with the virus, I was lost of hope when my doctor told me there is no cure for it but I keep thinking and thinking about my future, if I can have kids of my own well I am so grateful for my helper who get me cured with his herbal medicine, I go online in search of anything that can help me because I can’t deal with it forever so I found this Dr ehiaguna email on a Facebook of someone who was cured by him I quickly contact him for help and explain all my pain to him, he told me not to worry about it there is cure for real, I never believe until he send me the herbal medicine when I order for it and I have it within 4 days that is how I took the medicine for 2 week and the following week I go for test just to confirm I was 100% cured from this sickness what a miracle in my life I am so happy right now, you can also get in contact with him if you have such sickness through drehiaguna@gmail.com and also WhatsApp him +2348073908953. he can also help with this following sickness DIABETES CURE/EPILESY/HPV/CURE/LUPUS/HEPATITIS
ReplyDeleteGood day to you all am very happy to write this testimony to the whole world to see the great work of the great man named DR.ehiaguna I was down over since 1year but thank god am here to give this testimony for you all to see the great powers that is hiding on this earth I was once an HSV 2, but thanks to him that help me I was going through internet looking for cure when I see this man name ehiaguna I quickly email him If I can get help to grateful surprise to me he really do according to the post I see on internet this man ask me to provide some necessary things which he should be able to use for my cure, I did what he say and after everything, this man told me that after two weeks I will be cured, after that ending of the weeks i should go for test I did and I was very happy when I see my result but i don’t know how he did it but thank God for bring this man to me am very happy to see myself am HSV negative you can order now and get your cure on email: drehiaguna@gmail.com just call him for quick answer on his number +2348073908953, also contact him on this 1. HIV / AIDS 2. COPD 3. CANCER 4. ALS (Lou Gehrig's disease) 5. Hepatitis B6. HPV
ReplyDeleteBig thanks to Dr. Iyabiye who treated/cure my brother of chronic HEPATITIS B and Cirrhosis. My brother was diagnosed of the disease last year and we tried several antiviral medications but they were all to no avail. At a point my brother developed swollen stomach and loss of appetite, I went online out of frustration for a new medication and I came across this doctor’s recommendation. I reached out to him and my brother was cured after the completion of the medicine and tested negative at the hospital. Dr. iyabiye’s contact: call/whatsapp: +234-815-857-7300 and email: iyabiyehealinghome@gmail.com
ReplyDeleteI was haven herpes 2 on my genital area . I have had them for about 2 and a bit years. I am so scared what my mates are going to says if there should fined out i have herpes on my genital area and due to the virus my partnal broke up with me. I have been to the Doctors 9 times to get it treated. They all come back. I have been using Tee Tree Oil and Wartner (You freeze them at home) and they seem to be keeping the smaller herpes small but they can't seem to treat the larger ones. They don't get any bigger, but then they can't shrink as much. They get smaller a little part at a time. At least they are getting smaller! As soon as I see a new herpes appearing, then I treat it. At the moment I have been using Tee Tree twice a week and then using Wartner every 2 weeks. I was wondering if there was any other information about how to get rid of it. I am only a teenager and I hate it most when it get pi-chins me to scratch it, it get sweets when scratching it most times! I want to get rid of it so bad! DR. Odion website has been a huge help and has helped me realize a lot more about me and my family of genital herpes! so that was when I switch for natural remedy to see if there could be any help by herbal remedy, I search and I saw a great posts by Sarah devise Martha, Mignon Wright and shanttel Merritt on about the great herbal doctor that get them rid of there disease infection. and this great herbal doctor was called DR. Odion so that was when I contacted him for my own treatment and he prepared me some herbs which I takes for some couples of days, and I take it as he says before I am to no me and my family was perfectly cure for it and never experience it again. please friends if you have herpes virus and you really wants to get rid of it, please contact this great DR. Odion for herbal treatment and you will get rid of it. EMAIL. drodionherbalhome12@gmail.com OR WhatsApp number +2349019421176
ReplyDeleteTruly herbs have proven to be the best remedy for herpes and i want to share this to the entire public on how Dr OBOH cure me from herpes 1&2 with his herbs, I never believe it will work because the doctors keep saying there is no cure but i was desperate and needed to get this thing out of my body. I saw a comment online testifying how Dr. OBOH cures her from herpes and hpv and I contacted Dr. Oboh explains my problem to him and he prepares the cure and sends it to me through UPS, Which i use just the way He instructed me and thank God today I am a beneficiary of this cure. I went to my doctor for checkup after Two weeks of taking the herbs and I was tested Herpes 1&2 Negative and my doctor told me that the virus is completely gone from my system and he was very shock also and ask for his contact then i gave it to him and he also contacted him in need of other patients. So I will tell you all who are looking for a cure to his/her Herpes Virus, I will advise you to do a very good research about herbalist Oboh and see more about his good work and a lot of people are benefiting from him right now. He also cured my Uncle and his wife from HPV. Dr oboh heals with natural herbs. Please I urge you to contact him now through his email address: obohessn@gmail.com or WhatsApp him on +2348089281017 You can can thank me later
ReplyDeleteBEST NATURAL TREATMENT FOR HUMAN PAPILLOMAVIRUS (HPV) earning that you have HPV can be one of the most difficult experiences you go through in life. You may feel scared, sad or even angry – this is OK, and a completely natural part of coping with something that can be life changing.
ReplyDeleteIt will probably take a while for the news to sink in.
My name is Johnny Mary and i am from the United States.
I remember spending so much money buying drugs from hospitals hoping that i will be cured from HPV VIRUS, but all to no avail. I contacted so many doctors and they prescribe medicine for me which they indeed tried their best but was unable to provide for me a possible cure, luckily i saw a comment about a herbal doctor, (Dr.Ogberaese) online.
I then contacted him (Dr.Ogberaese) through his email, After much chat and enquiry with the doctor, i decide to take a leap of faith because i have nothing to loose.
To my greatest surprise, Dr.Ogberaese prepare a medicine and send me a Herbal Medicine through FEDEX courier Service, and he gave me guidelines on how am to take it. I followed all procedures as instructed, and after 2 weeks of taking it i was cure from HPV VIRUS his medicine is legit and it is real. I just want to encourage all individuals out there living with HERPES , ITCHY SHINGLES , Genital Herpes, HSV1&2, HIV/AIDS/ HPV, COPD, CANCER, Hepatitis b, Lupus, PCOS, Kidney failure, Lung cancer and alot more. That there is still a huge chance that you can get cure only with the help of dr Ogberaese. kindly contact him via email: drogberaese54@gmail.com or whatsapp: +2348073818653
Hello viewers, I have been a victim of the Herpes virus for 11months. One day i was in a mall when I meant a friend of mine that once knew that i was suffering from same problem with hers and she introduce me to a man called Dr Okorom that have cure her Herpes virus with the help of his traditional medicine I contacted him and he gave me the traditional herbal medicine to drink and after drinking it with his prescription he told me that after 2 weeks I will see the result of his traditional herbal medicine and today I am happy to say that Dr Okorom have used his traditional herbal medicine to cure my Herpes virus, and now I am happy to be alive life again today with my family, I am married with 2 kids, to all that feels my pain and will need to know more about this great traditional doctor here is his contact: dr.okoromspellhome@live.com or WhatsApp him via +33 6 05 81 04 88 i am sure he is the solution you have been waiting for so don't let this opportunity pass you by okay.
ReplyDeleteI'm so Happy to write this article because I know it will help a lot of people who are suffering from Herpes. I am here to testify about the wonderful and most safe cure for herpes . I was positive to the deadly Virus called herpes and I lost hope completely because I was rejected even by my closest friends. I searched online to know and inquire about a cure for herpes and I saw testimony online on how Herbalist called Dr Osamu who cured so many people from Herpes virus and other similar diseases. I decided to contact the great herbalist because I know that nature has the power to heal everything. I contacted him to know how he can help me and he told me never to worry that he will help me with the natural roots and herbs. After 2 days of contacting him, he told me that the cure is ready and he sent it to me via UPS and it got to me after 4 days. I used the medicine as he instructed (morning and evening ) and I got cured. it's really like a dream but I'm so happy that's the reason i decided to also add more comment of Him so that more people can be saved just like me and if you need his help, contact him via Email: dr.osamuherbalremedy@gmail.com or WhatsApp:+2349012406016
ReplyDeleteBattling with any health related issues or infection is not the end of your life, why not contact a herbal practitioner for cure Dr Abolo has herbal remedies and permanent solution for all your health related problems.I recommend him to you today only because i have also used his herbal medicine and it worked perfectly on my health problem with out side effect, you can actually save yourself from giving your hard earned money to drugs than cannot cureyou if only you can contact Dr Abolo today for your permanent cure and herbal products . Please help me share this post to save yourself and your love ones.Dr Abolo is specialize in these areas,Permanent herbal supplements for anxiety and depression,HIV/AIDS, Diabetes, Epilepsy, Blood, Cancer, HPV, ALS, herpes etc. Email: draboloherbalhome@gmail.com also call or whatsApp him on +2347044725611
ReplyDeleteI want to give a testimony on how I was cured from herpes ii virus after using Doctor Patrick liquid herbal medicines for one month only, i found about Doctor Patrick on newspaper, I had to take his email and phone number and then contacted him, I explained everything to him and he assured me that he can help me and I will be free from this infection forever. He sent me the medicines and I started using according to his instructions, after two weeks of using the medicines, I saw great changes, I continued using the medicine until I used it all for one month, I was cured totally, no more symptoms and I went for another diagnosis, the Doctor gave me my test result and it came out negative, I want to thank God for making this come true and I want to thank Doctor Patrick for what he has done for me, contact this herbal doctor on herbalmedicalhome@gmail.com and whatsApp number is +2348021312463.
ReplyDeleteI've been treating herpes virus for several years with different medications until I saw a post on how a young lady got cured from herpes, Out of desperation I decided to contact him with little or no hope of a solution after taken his herbal medications reluctantly to my biggest surprise I tested negative, God bless you Dr ubarlo drubarlohome@gmail.com or Whatsapp +2348119508814 for his wonderful work
ReplyDeletefew week ago I felt some pains and I went to the hospital my doc told me I had Herpes about 1 year ago and I need to start the treatment early, he gave me some medicine to be taking and I told him no I’ll not, because I hated taking medicine when I won’t not see cure for the purpose. After I got home I started getting worried searching for strong advice and I found valid natural treatment online a lot of people says they got herpes cure from DR ehiaguna and I contacted DR ehiaguna that same day I purchase his cure online, after two weeks of taking the herbel treatment i got cured totally. i tested negative all thank to DR ehiaguna you can also reach him on his email: [drehiaguna@gmail.com ] or message him on WhatsApp +2348073908953 God bless you
ReplyDeleteI was depressed when the doctor told me that I have been diagnosed with Herpes disease… I thought about my Family, I know my Family will face a serious problem when I'm gone, I lost hope and I wept all day, but one day I was searching the internet and I found Dr.obudu' contact number. +2349023428871 I called him and he guided me. I asked him for solutions and he started the remedies for my health. Thank God, now everything is fine, I'm cured by Dr.obudu herbal medicine, I'm very thankful to Dr.obudu and very happy with my hubby and family. email him on drobuduherbalhome@gmail.com or you can also reach him through WhatsApp number+2349023428871 also visit hes websitehttps://drobuduherbalhome.wixsite.com/welcometoobuduherbal or visit his facebook page https://www.facebook.com/DR-OBUDU-101779795066025/
ReplyDeleteHe can also cure so many sickness
{1}HIV And AIDS
{2}Diabetes
{3}Epilepsy
{4}Blood Cancer
{5}HPV
{7}ALS
{8}Hepatitis ,.,.,.,.
months ago I felt some pains and I went to the hospital my doc told me I had Herpes about 1 year ago and I need to start the treatment early, he gave me some medicine to be taking and I told him no I’ll not, because I hated taking medicine when I won’t not see cure for the purpose. After I got home I started getting worried searching for strong advice and I found valid natural treatment online a lot of people says they got herpes cure from DR ODUDU and I contacted DR ODUDU that same day I purchase his cure online, after three weeks of taking the herbal treatment i got cured totally. i tested negative all thank to DR ODUDU you can reach out to him through his email: [dr.oduduherbalhome@gmail.com ] or message him on WhatsApp +2348101571054 stay safe and bless you
ReplyDeletefew week ago I felt some pains and I went to the hospital my doc told me I had Herpes about 1 year ago and I need to start the treatment early, he gave me some medicine to be taking and I told him no I’ll not, because I hated taking medicine when I won’t not see cure for the purpose. After I got home I started getting worried searching for strong advice and I found valid natural treatment online a lot of people says they got herpes cure from DR.IMOUDU and I contacted DR.IMOUDU that same day I purchase his cure online, after two weeks of taking the herbel treatment i got cured totally. i tested negative all thank to DR.IMOUDU you can also reach him on his email: [DR.IMOUDUHEALERTEMPLE@GMAIL.COM ] or message him on WhatsApp +2348109609753 God bless you
ReplyDeleteHELLO everyone! Still don’t know the right words to express my Gratitude to the Great DR David After been diagnose with the #herpes for the passed 1 years, i was given so many health prescription and advice with no improvement, I totally lost hope, until i found many testimonies of Great DR David in an online research Like anybody would be, i advice anyone that is living with herpes can also contact him today, because he has the cure to virus problem contact him on WhatsApp +2348103442287
ReplyDeleteOr his Email: drdavidherberhome@gmail.com
1…ALS CURE/DIABETES CURE/EPILESY/HPV CURE/LOOSE WEIGHT AND BODY/EX-BACK/HEPATITIS/
THANK YOU DR David FOR YOU GOOD WORK IN MY LIFE..
https://www.facebook.com/Dr-David-Herbal-Home-109272270791218/
I still cant believe that my herpes is gone after two years of suffering. Thanks to Dr Momoh who cured my herpes with his herbal medication I never thought I will ever be heal again, I was a herpes positive two years ago and I have try so many medication so I can be free of this dearly disease but nothing work out, so one day I go on a research on the internet where I saw someone given testimony on how Dr Momoh help him to cure his herpes virus with his herbal medication, so I said to myself it also the same problem am having so I have to also contact the herbal doctor Dr Momoh on his email which the man recommended to anyone who might also need his help, Wholeheartedly am so grateful to this man as he help me with the cure and make me a happy man again. Anyone out there who might be facing same problem should kindly contact Dr Momoh as is know he will help you with all your problems, contact him through his email dr.momoh9@gmail.com, call or WhatsApp him +2347083724098
ReplyDeleteThere are Illness that drugs and injection can't cure ,I have seen the great important of natural herbs and the wonderful work they have done in people lives , I have read peoples testimonies online on how they were cured of HERPES ,CANCER, FIBROID, HPV, LUPUS, DIABETES,INFERTILITY, PENIS ENLARGEMENT LOW SPERM COUNT etc by Dr. Ehizele herbal medications , so I decided to contact the great doctor ,because I have spent a lot in hospitals and clinics , so I have no choice than to try herbal medications , I have diagnosed with hiv , since 2010, I lost hope of been cured , until I contacted this Dr and he sent me herbal mixture through the ups delivering service , which I drank for 14 days and I went to test after 14 days , I went for a test just to discover that I am free from hiv, I was so happy and it was like a magic to me. I like to let the whole world know that there is a cure for hiv , am a living testimony of Dr Ehizele herbal medications,its real and it works
ReplyDeleteContact Dr Ehizele with the info below and get cured from different types of viruses and diseases
*WhatsApp* +2347089384319
*email* ehizeleherbalhome@gmail.com
Powerful Herbal treatment is 100% guarantee for HSV cure, the reason why most people are finding it difficult to cure HSV 1 or 2 is because they believe on medical report, drugs and medical treatments which is not helpful to cure HSV and hasnít proved any sign of helping. Natural roots/herbs are the best remedy which can easily eradicate herpes forever. I never believed it until I was helped and cured of my 16 months genital herpes with natural herbal medicines from Dr Aza. Where other medical prescribed drugs and treatments failed, Dr Aza natural herbs helped saved me from Genital herpes permanently and i am so grateful for this. You can also get help from this great and powerful African Herbalist Dr Aza or you can also contact Dr Aza through his email :drazaherbalcenter@gmail.com or WhatsApp him via: +1(315)7951518 , you can also visit his website on: www.drazaherbalcenter.com
ReplyDelete100%Natural herbal remedies for women
ReplyDeletePelvic inflammatory Disease (PID), is an infection of a women’s reproductive organ. It is caused by bacteria that travel up the reproductive tract. PID can result in inflammation of the uterus, ovaries, and fallopian tubes which could lead to infertility and ectopic pregnancy. PID can also lead to long-term health problems If left untreated, and it can even be life-threatening.
Here is the Symptom of PID:
1. Unusual or heavy vagina discharge
2. Abnormal Uterine Bleeding
3. Lower Abdominal pain
4. Bleeding between period
5. Black pain
6. Painful sexual intercourse
7. Painful frequent urination.
Interested people to have it contact me (+2349065326267) inbox me dr.olutaspellcaster@gmail.com or comment below!
I’d recommend using Dr. Utu Herbal Cure topically for instant pain and itch relief as well as accelerated healing of lesions and permanently stopping oral and genital herpes virus outbreaks. I have tried just about everything from acyclovir suppressive therapy to different natural oils, extracts, and other natural methods, some of which are EXTREMELY painful and exacerbate the problem (i.e. apple cider vinegar!). While vitamin E oil and suppressive therapy worked well for me, when I became pregnant I went back to trying to find a herbal cure. I was using vitamin E oil topically for a while but it was thin and difficult to use and only seemed to prevent further outbreaks rather than getting rid of it. I contacted Dr. Utu Herbal Cure through my friend. To my surprise, I could tell my outbreak was starting to heal within only a few hours! No more itching or pain! Dr. Utu Herbal Cure that I used was liquid herbs in bottles, so it was very easy to use. It simply whiffs, but it works so I don’t care! The best part is I successfully delivered a herpes-free beautiful daughter without further medications. Anyone who has tried Dr. Utu Herbal Cure knows just how quickly those treatments can add up. So give it a try! Anyone can reach Dr. Utu through
ReplyDeletedrutuherbalcure@gmail.com
+2349072733661
I am really happy that i have been cured from (HERPES SIMPLEX VIRUS) with the herbal medicine of Dr MOMOH , i have been suffering from this disease for the past 3 years and 4 mouth without solution until i came across the email of this doctor who have cure so many people with his herbal medicine, i also choose to give him a chance to help me and my husband, he told me what to do and i kindly did it, and he gave us his herbal medicine and direct me on how to use it, i also follow his instructions for use and he ask us to go for a check up after 1 week and 5days which i did, to my greatest surprise our result came out as negative, we are really happy that there is someone like this doctor who is ready to help anytime any day. To all the readers and viewers that is doubting this testimony, stop doubting it and contact this doctor if you really have one and see if he will not actually help you. i am not a stupid woman that i will come out to the public and start saying what someone have not done for me and i know that there are some people out there who are really suffering and hurting their family just because of these diseases so you can Email him on dr.momoh9@gmail.com OR WHATSAPP him on +2347083724098 he also told me that he has cure for these diseases listed below . HERPES SIMPLEX VIRUS. .DIABETES . CANCER .HEPATITIS .HIV/AIDS Thank you for your time
ReplyDeleteI'm recommending Dr Okuofoh to everyone who has the herpes simplex virus to get the cure from him. I was diagnosed with genital herpes in 2020 and I have been searching and asking questions to see if I could get something to cure the disease because I did not believe what the doctors say that no cure is found yet. I came across a comment on Youtube and the person testify how she was cured of herpes after using Dr Okuofoh herbal medicine. I quickly contact Dr Okuofoh and explain my problem to him and he prepares the herbs and send it to me through UPS and gave me instructions on how to use it and tell me to go for a checkup after usage which I did after two weeks of taken the herbal medicine and my result was NEGATIVE. I waited another month and retested the result was still NEGATIVE and my doctor told me that am completely free from herpes. Am so happy and grateful to Dr Okuofoh for what he has done for me and I will continue to share this with people out there to know that there is a herpes cure can contact Dr Okuofoh by email and Whats App to get the cure from him. Email: drokuofohherbalhomehealing@gmail.com
ReplyDeleteCall or WhatsApp +2349050141449.
I'm here to testify about the great work Dr Ede did for me. I have been suffering from (HERPES) disease for the past 3 years and had constant pain, especially in my knees. During the first year, I had faith in God that I would be healed someday. This disease started circulating all over my body and I have been taking treatment from my doctor, few weeks ago I came across a testimony of one lady on the internet testifying about a Man called Dr Ede on how he cured her from Herpes Simplex Virus. And she also gave the email address of this man and advised anybody to contact him for help for any kind of sickness that he would be of help, so I emailed him telling him about my (HERPES Virus) he told me not to worry that I am going to be cured!! Well I never believed it,, well after all the procedures and remedy given to me by this man few weeks later I started experiencing changes all over me as Dr Ede assured me that I will be cured, after some time I went to my doctor to confirmed if I have be finally healed behold it was TRUE, So friends my advise is if you have such sickness or any other at all you can contact Dr Ede via email(dredespellcasters@gmail.com) Or WhatsApp him (+2347064290546)
ReplyDeleteI still don’t know the right words to express my gratitude to this great man Dr. Momoh. After been diagnosed of HERPES SIMPLEX VIRUS in 2months ago, i was given so many health prescription and advice with no improvement, I totally lost hope, until i found testimonies of Great Dr. Momoh online research and on Facebook, Like anybody would be, I was very skeptical about contacting him, but i later did and he opened up to me and told me what was involved and he started the remedies for my health. Thank God, i was cured from herpes by the herbal medication I received from him. I never thought that herpes can be cured from the bottom of my heart I'm truly grateful, i pray you have long life so you can help many more people on earth with your herbal medical support, You can Email him via email dr.momoh9@gmail.com or for easy and fast communication you can also call. or add him on whats-app with this mobile number +2347083724098 , one thing i love most about DR momh is honestly, and he is very polite with his patience, everything he told me was what he did, and his herbal medicine are very affordable
ReplyDeleteA GREAT THANKS TO DR.JACOB FOR CURING ME FROM GENITAL HERPES I AM SO HAPPY TO GIVE THIS TESTIMONY ARE YOU SUFFERING FROM THIS SICKNESS HERE IS DR WHO CAN HELP
ReplyDeleteI can’t believe my genital herpes is really cured, oh is by this time last year I start feeling bad about my life, I feel pain everyday of my life am very happy now that am really cured I couldn’t have do this on my own I wish is not God that help me with my helper I was searching the internet about this sickness last 3month when I found about great doctor wealthy, the man that keep his words I write the man email about my problem immediately I get a reply from him asking me to fill a form which I immediately did and send back to him after some mins he reply me that he have work on my cure that I need to provide some materials, which can enable him to work on my cure which I did on the next day of it, after some hours he inform me that he have getting the things needed for the cure and he is about to go on with the curing spell he called me again after 50mins that he is done with the cure that I should check my body and also go for test I cant believe I was negative a big thanks to him am very happy now with my family you can also get your self cured too from this sickness by contacting him through his email: drjacobherbalhome2@gmail.com WhatsAPP +1 (336) 962-8303 He also have a herbal cure for 7 other DISEASES;
1.HIV
2.SHINGLES
3.VIRAL HEPATITIS
4.INFLUENZA
5.IMPOTENCE,
6.BARENESS/INFERTILITY,
7.ANTHRAX
8 HPV
Contact him today and you will have a testimony…Good luck!