"I wasn't really thinking PE at first," they explained to me, "but after I saw the incomplete RBBB on the ECG, I sent a D-dimer." The D-dimer, of course, came back trivially elevated, and the CT had been ordered.
Ah, the scourge of the IRBBB. It typically take the appearance of an rSR' pattern in V1 and V2 with a narrow QRS, although the AHA takes a dim view of this colloquial definition.
This seemingly "hard" element of evidence, however, can be surprisingly malleable!
I cured the patient's IRBBB!
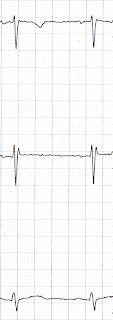
The patient was already off at CT, so I looked at the ECG myself. It looked pretty darn normal, except for the right-precordial leads:
V2 shows an rSR' pattern, clearly.
The patient returned from CT scan, and I awaited the results. In the meantime, however, I re-interviewed an examined the patient, and convinced myself that she was low risk for all of the "bad actors." The IRBBB stuck in my craw, however, and after some fiddling around, I aquired a new ECG.
Sweet. It's not up there with sinking a difficult tube, or threading a pacer wire, but it makes for a cleaner chart!
What did I do?
I put V1 and V2 where they are supposed to go.
For a fuller explanation of the background here, please check out The most difficult step in obtaining an ECG. It's a post I wrote for paramedics about the importance, as well as the common difficulty, of placing the precordial leads in the correct locations. It's written in a conversational and witty tone, with plenty of illustrations - you'll like it!
Suffice it to say, though, that V1 and V2 are usually placed far too high on the chest. This produces a number of artifacts, including pseudo-infarction patterns and, yes, IRBBB.
I took a picture (with the patient's knowledge and permission - she believes in education!) of the actual lead placements on the patient's chest. The electrode wires are attached to the proper locations, at the 4th intercostal spaces, just to the right and left of the sternum.
 |
| Thank you Ms Anonymous! |
The Bottom Line
Learn where to put the leads yourself.
If the diagnosis is going to rely critically on the ECG, you ought to check out where the electrodes were placed by the nurse, tech, or paramedic. Certainly, if there are abnormalities isolated to the precordial leads you should go back and do this, especially if the ECG doesn't match the patient's age or presentation.
BONUS QUESTION: For major extra points at the "Port, tell me what electrophysiologic diagnosis may rely on placing V1 and V2 higher than usual.
(Answer can be found by checking my self-aggrandizing link.)
*******
Added post-publication.
Mr Várhegyi points out a similar example, elsewhere on the web, of an IRBBB. Oddly, that example seemed to show some QRS prolongation in V2 that was not appreciated in the other leads.
 |
| Source |
So, I took another look at my patient's initial ECG:
Darned if it doesn't seem to also have an isolated, minor (< 0.02 seconds), QRS prolongation in V2.
I'm going to defer providing an explanation until I have some idea about why this occurs, or even declaring that this is a reliable feature of improperly placed precordial leads. But it's apparent in these two examples. I'll look into it - anyone else with a better idea write in!